No 29 - One reason why GP's get a bad name in acute medicine
TLDR
GP referrals letters to acute clinicians should start with a clear reason for the referral, rather than starting in the traditional way with the clinical history and the reason at the end. This one minor change could improve relations between acute clinicians and GPs.
https://en.wikipedia.org/wiki/The_House_of_God
I am coming to the end of my time in General Paediatrics and I have nearly done my last clerking shift in Paeds CDU (Clinical Decision Unit). Between these CDU shifts and my previous ED rotation, I have read an awful lot of GP referrals letters in the last 8 months and seen an even larger number of GP referrals.
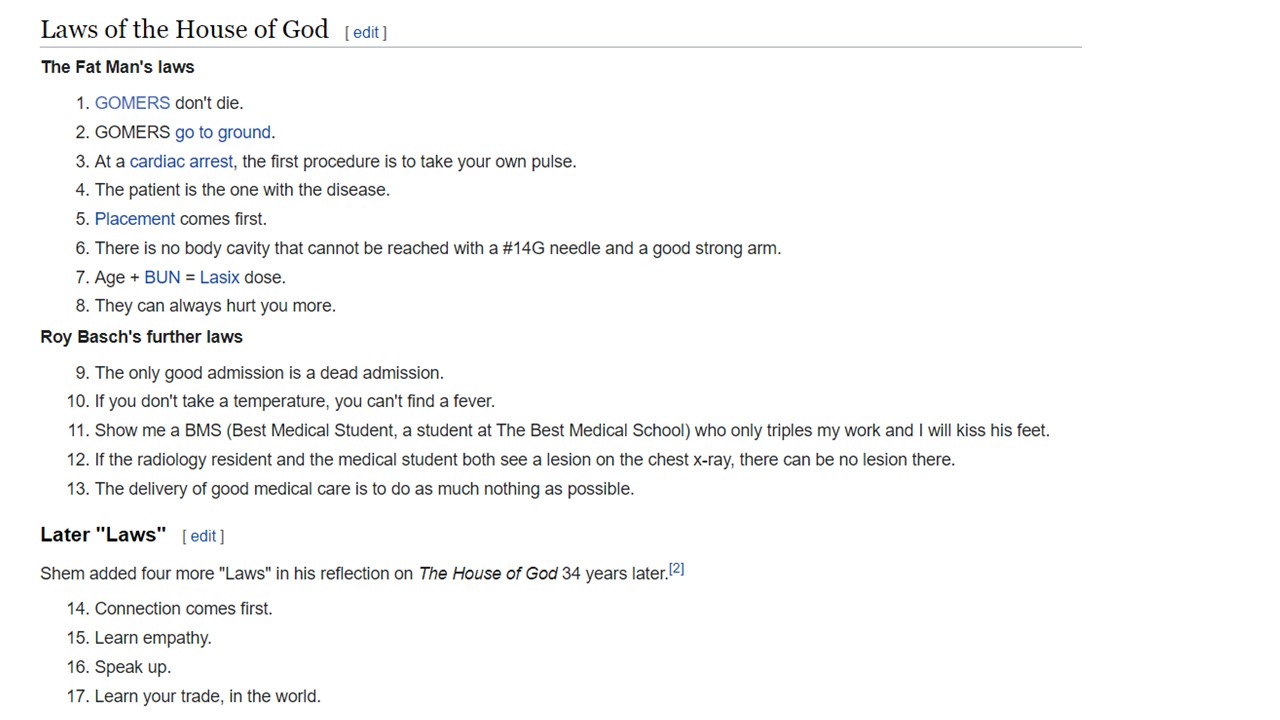
GP’s often get tarred with the same brush, and as a cohort, we often get a bad rep from hospital staff. Mostly, I think this can be explained by Rules 9-13 of the House of God (see above). Even dedicated medical professionals don’t always enjoy being given more work. GP referrals are roughly 1/3 or 1/4 of every patient seen acutely and therefore, it looks like GPs are creating work for the reviewing clinicians.
One way of letting off this frustration at having to do “extra work” is to bash the person “creating work” for you. Hence, GP bashing. It can be the same tribal mentality between almost all hospital specialities at some point during a busy shift.
Firstly, lets exclude all of the patients who turn up without a GP letter and just say “my GP told me to come”. We all know this is slightly frustrating.
Next, we need to just point out how frustrating it is to only receive a GP “letter” that is a print out of their recent consultation. Sometimes, with an addendum of “tried to call RMO but couldn’t get through, so I have sent the patient urgently…”
Even worse than a GP print out, is an NHS 111 print out! The pages and pages of barely English algorithmic nonsense are almost useless. I don’t know who wrote those algorithms or print outs but they have very strange grammar (and before anyone points it out, yes I know my English skills aren’t amazing). These statements seem to have all the filling at the beginning and then the key words at the end, which just makes them very difficult to read quickly. For example, “the patient attended, they did not report that they have any chest pain”. Instead of “Chest pain - no”. If anyone from NHS 111 or Out of Hours GPs is reading this, could you please make this change? Simplify your documentation.
However, the worst and most frustrating thing about GP referrals, is when there is no clear indication for the referral in the letter! In layman’s terms they have not written why they want you to see the patient?
I honestly believe, just 1 slight change in how GPs refer could make a huge difference. Even if you still just send a GP consultation print out. At the top of the entry, or the start of the letter just include the following:
“Dear Colleague, Could you kindly see Miss X because …”
I think they have red flags requiring urgent investigation;
they have red flags requiring urgent inpatient admission;
I am worried about this symptom and would value a second opinion;
the NICE guidance Y suggests they need urgent review by your speciality;
I am not too sure what is going on and think they would benefit from a few hours of observation;
I need your help. Please do the needful.
Putting this at the top of the letter is also good psychology because it makes it quick and simple for the receiving clinician to work out what you want and they can then read the rest of the letter if they want additional information. This reduces the frustration of having to read more stuff that is not necessarily relevant to what you want to know.
I know this sounds like additional work and a change in practice for some people but it would really help the hospital clinicians and would improve the relationship between the hospitals and the GPs.
Clearly asking for help in a professional manner would hopefully produce respect for a referral well done. It would also help you clarify in your own mind what is going on and what you expect to be done by the hospital, and hence, what you can tell the patient to expect. I would like to think that you the GP, the acute clinician and the patient all win from this one, simple change.